 Listen to this story.
Listen to this story.
Librela
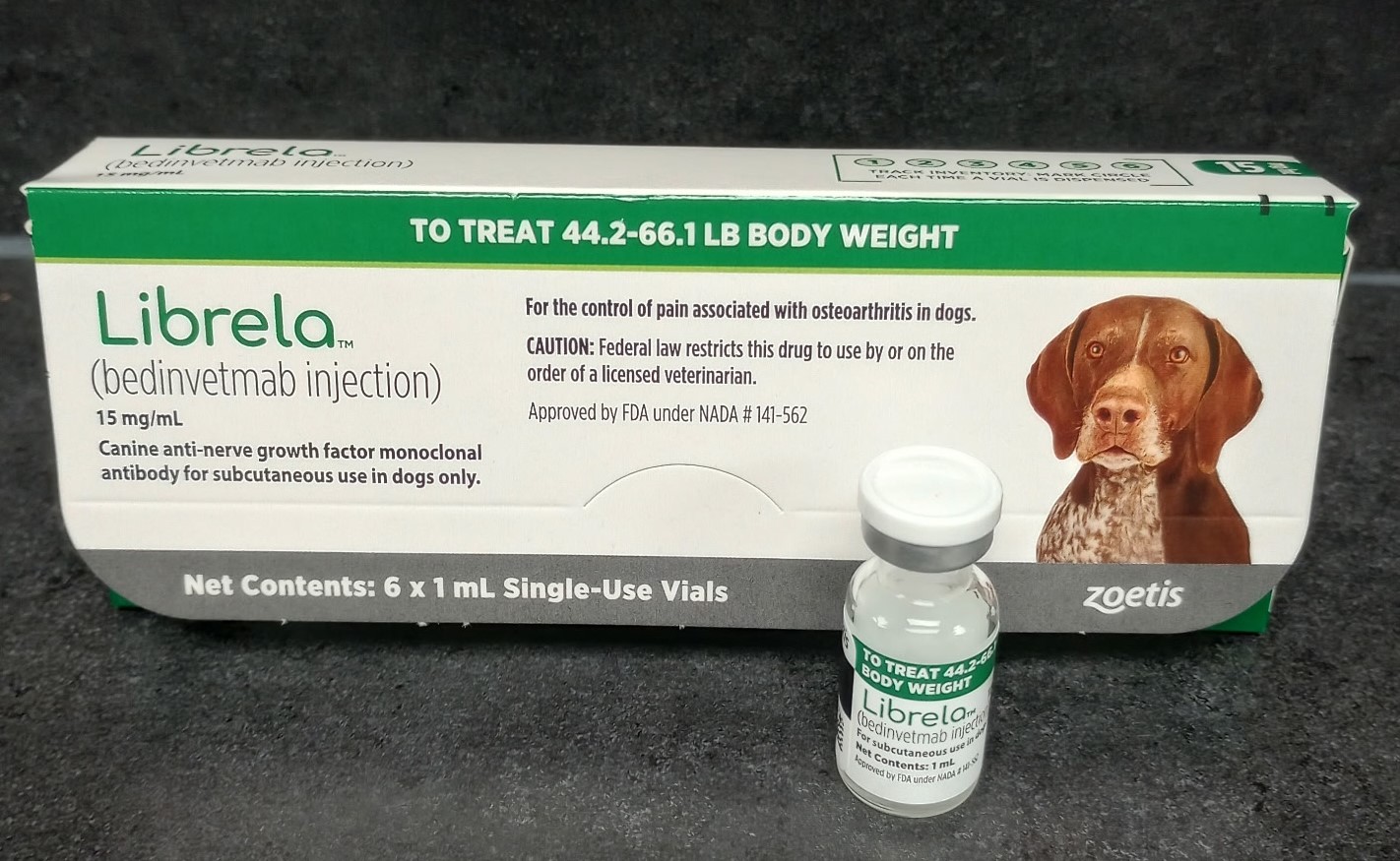
Photo by Dr. Steve Miletta
First introduced in 2021, Librela is given as a monthly injection to treat osteoarthritis in dogs.
Discussion in the veterinary community about the safety profile of a popular new osteoarthritis drug for dogs is continuing with vigor, stoked by three research papers — two backed by the drug's manufacturer, Zoetis — that give contrasting impressions of the risk of side effects.
Zoetis maintains that the vast majority of patients receiving the injectable treatment, branded Librela, have positive experiences and that associated adverse events are rare.
The most recent study, published May 9 in Frontiers in Veterinary Science and led by an independent orthopedic specialist in the United Kingdom, found that Librela caused a disproportionately high incidence of musculoskeletal side effects in dogs compared with six other types of treatment.
The research paper also suggests that rapidly progressive osteoarthritis (RPOA), a severe and debilitating condition, may be a side effect of Librela.
By contrast, another study, published on March 24, also in Frontiers in Veterinary Science, concludes that dogs treated with Librela were less likely to experience adverse events than dogs treated with meloxicam, a nonsteroidal anti-inflammatory drug (NSAID). Zoetis helped design that study, which was conducted by a consultancy paid by Zoetis.
On April 24 in the same journal, Zoetis gave its tally of adverse events associated with Librela, concluding that the most common are "rare" or "very rare," as defined by the Council for International Organizations of Medical Sciences, a Swiss nongovernmental organization.
The active ingredient in Librela is bedinvetmab, a monoclonal antibody that blocks nerve growth factor (NGF), a protein associated with the formation of nerves and pain generation. Zoetis also makes a bedinvetmab-based drug for cats, called Solensia. Attention among researchers and regulators to safety questions has been more on Librela, perhaps since clinical signs of osteoarthritis are harder to identify in cats and reported less frequently by owners to veterinarians.
NGF-blocking monoclonal antibodies have not been approved for use in humans because they were found in clinical trials to cause RPOA in some human patients.
Zoetis maintains there is no risk of RPOA in canine and feline patients, and Librela and Solensia have been approved by regulators around the world. The products were first introduced in 2021, in Europe, and have since been rolled out to countries such as the United States, Canada, Brazil, Japan and Australia (the last where it is branded as Beransa).
Amid the sale of millions of doses of the products, thousands of adverse event reports have been submitted to regulators encompassing suspected side effects such as lethargy, neurological disorders like a loss of coordination (ataxia), renal and urinary disorders, and disorders of the digestive tract, like vomiting. In December, the U.S. Food and Drug Administration distributed a "Dear Veterinarian Letter" to practitioners about side effects of Librela. The agency recommended that Zoetis update the drug label to list them, which the company did in February.
Musculoskeletal side effects in focus
Talk of the efficacy and safety of Librela and Solensia abounds on the message boards of the Veterinary Information Network, an online community for the profession and parent of the VIN News Service. Many veterinarians recount positive experiences with the drugs. Others express concern about side effects, some referencing the most recent paper looking at musculoskeletal adverse events in dogs.
The idea to pursue that research came from its lead author, Dr. Mike Farrell, an orthopedic specialist in Glenrothes, Scotland, after he noticed severe joint degeneration in a young Labrador retriever patient that had received six Librela injections.
Farrell and fellow researchers examined a European Medicines Agency (EMA) pharmacovigilance database from May 20, 2021, to Dec. 31, 2024. According to the published study, they found reports of musculoskeletal adverse events to be about nine times as common in dogs treated with Librela than the combined total of six comparator drugs — a disparity the authors describe as "striking."
Adverse events included ligament and tendon injury, fracture, abnormal tissue growth (neoplasia), arthritis caused by infections (septic arthritis) and arthritis in at least five separate joints (polyarthritis). The six comparator drugs were carprofen, meloxicam, firocoxib, robenacoxib, enflicoxib and grapiprant.
The researchers noted that a recent FDA review also identified a disproportionate incidence of certain side effects in dogs treated with Librela compared with other drugs.
Zoetis maintains there are limitations in the study led by Farrell and has written to Frontiers in Veterinary Science to express its concerns, the company's chief medical officer, Dr. Richard Goldstein, told VIN News. Goldstein also has written a letter to veterinarians that is critical of the Farrell-led research.
Among Goldstein's assertions is that, because Librela and the comparator drugs were released commercially at different times, it is "inadequate to compare adverse event reporting of different classes of therapy with different maturity in the market."
In an interview by email, Farrell disagreed, noting that the analysis encompasses a period when Librela and the six comparator drugs all were commercially available.
Dr. Dawn Boothe, a retired Auburn University College of Veterinary Medicine professor and former director of its clinical pharmacology laboratory, said Goldstein's argument as to a limitation seems reasonable because the length of time a treatment has been available might influence whether users bother to report adverse events. "As the 'newness' wears off and adverse events become 'old news,' the likelihood of reporting decreases," said Boothe, who now produces drug information resources for VIN. Moreover, she said, the level of concern associated with a certain type of adverse event — and likelihood that it will be reported — could change over time. For example, she said, "We were not really looking for musculoskeletal outcomes until more recently."
The Farrell-led research team reviewed adverse events going back to 2004 to check whether reports on the comparator drugs surged, then tapered, following launch. The authors concluded that there was no such trend. Boothe suggested that looking back 20 years at reports may not be entirely sufficient, noting that two of the comparator drugs, carprofen and meloxicam, were introduced more than 25 years ago, in 1997 and 1998, respectively. Some of the other comparator drugs are similar NSAIDs, she said.
In the assessment of Dr. Mark Rishniw, an adjunct associate professor at Cornell University and director of research at VIN, the study by Farrell and team appears sound overall. One possible point of criticism, he said, is that the study is based only on reported adverse events. "There would be a clear bias because they were selecting from a pharmacovigilance database rather than just random events," Rishniw said.
Farrell countered that analyzing data from a safety monitoring database is a globally accepted standard of surveillance for commercially available drugs. "The purpose of such a study is to characterize the nature of spontaneously reported adverse events, not to calculate their frequency in the general population, which would require a completely different study design," he said.
Could RPOA be a side effect of Librela?
In a separate part of the study, the researchers analyzed 19 cases of patients that displayed severe signs after receiving Librela, one of which was the Labrador retriever that inspired the study. (The dog was euthanized due to intractable pain.) The case studies, drawn from around the world and reviewed by an 18-member expert panel, concluded there was a "strong suspicion of a causal association" between Librela and "accelerated joint destruction."
The study authors contend that the absence of RPOA as a formal diagnostic term in veterinary medicine represents a weakness of the profession's pharmacovigilance system and calls for the condition to be included in the Veterinary Dictionary for Drug Regulatory Activities, a list of standard clinical terms.
Goldstein at Zoetis said RPOA is not a possible side effect of Librela because, he maintains, the term refers to a condition affecting humans only. "RPOA is a very, very specific human term that has very specific criteria for people," he told VIN News.
At the same time, Goldstein said Zoetis is open to the possibility that an "abnormal progression" of osteoarthritis could be a side effect of Librela — albeit rarely, he added, in the context of the approximately 28 million doses of Librela sold to date.
Dr. Tina Wolfe, an orthopedic surgeon in Ohio, described the severe nature of the joint destruction seen in the 19 case studies as "eye-opening."
"Although a single study may not definitively prove causation, these adverse events cannot be easily explained by other causes," said Wolfe, who also is a consultant at VIN, serving as a subject-matter expert on its message boards. "Even if the incidence is low, any occurrence of such serious and unusual complications should get our attention and stimulate further research."
Goldstein said Zoetis is engaging in studies to better determine what a natural progression of osteoarthritis looks like in dogs compared with humans.
Other paper suggests Librela safer than meloxicam
Of the other two recent studies, one found that dogs given Librela at any of eight veterinary participating practices in the U.K. between March 2023 and March 2024 experienced substantially fewer adverse effects than dogs given the NSAID meloxicam. The study received funding from a consultancy founded by the study's lead author, Dr. John Innes. The study authors disclosed that the consultancy had a paid contract with Zoetis and that Zoetis provided input on the study design and agreed to the final design.
Of 52 dogs given Librela, four had adverse reactions: Two exhibited lameness, one had excessive thirst (polydipsia) and one developed a skin cyst. Of 49 given meloxicam, 17 had adverse reactions, including eight with digestive tract disorders such as diarrhea and vomiting, three with ataxia and three with lameness.
"Overall, from a safety perspective, this study demonstrated a lower adverse event rate in dogs treated with bedinvetmab compared to those treated with meloxicam during a 56-day treatment period," the authors state, referring to Librela by its active ingredient. "However, it must be acknowledged that this study lasted for only 56 days, which limits the safety data conclusions."
Dr. James Fingeroth, a retired veterinarian in New York and VIN orthopedic surgery consultant, called for research that looks more closely at the seriousness of adverse events rather than their frequency alone.
"Since many dogs will likely benefit from Librela (and cats, from Solensia), I suspect both veterinarians and clients will continue to endorse it, with a few clients ending up devastated because their pet had one of the really bad adverse events," he said by email. "I expect it will come down to the incidence of those really catastrophic events and how veterinarians and clients will respond to that risk."
Ideally, Boothe said, further studies focused on severe joint degeneration would include control animals that did not receive Librela. "But mainly what we need is a large enough sample size in a clinical trial comparing joint destruction like this in animals receiving an NSAID or other drug versus Librela. The study by Innes et al. is a start, but the sample size is too small if we acknowledge the very low frequency of this adverse event in dogs receiving Librela."
Contention over risk assessment method, reporting accuracy
The paper by Farrell and colleagues also criticizes a tendency by Zoetis to assess risk by weighing the number of adverse event reports against the number of doses sold. That's problematic, the authors maintain, because serious cartilage and bone degeneration often occur before clinical signs become apparent and may therefore go unreported. The authors note that the FDA does not use sales-based prevalence estimates for that reason.
Goldstein agreed that sales-based estimates can underrepresent the prevalence of adverse events but said they nevertheless provide a useful guide. "If you have 100 people using a drug and you've 10 reports, that's different than if you have 10 reports out of a million people using a drug," he said, noting that the FDA's European counterpart, the EMA, uses patient numbers to assess the prevalence of adverse events.
The Farrell-led paper also questions how accurately Zoetis recorded some adverse events to the pharmacovigilance database that had been submitted to the company by veterinarians. In one of multiple cases cited by the authors, an orthopedic specialist in the U.K. reported a Labrador with mild elbow dysplasia had experienced severe joint degeneration after receiving 23 doses of Librela. The doctor reported the event as an unusually rapid progression of osteoarthritis and identified Librela as a possible cause. Zoetis subsequently filed the event as "not serious" and changed the patient outcome from "ongoing" to "recovered/resolving," the study authors wrote. Of the 19 case studies, nine had translational errors, according to the paper.
The apparent discrepancies provoked a submission to the journal of a commentary by two veterinarians not on the Farrell-led study team who expressed concern about how adverse events are recorded in pharmacovigilance databases and called for a more stringent and transparent reporting process.
Goldstein said original submissions can appear differently in Zoetis' reports because the company must enter information within rigidly defined categories that limit room for nuance. Moreover, he said, the process can be complicated by the submission of multiple reports about the same patient from different sources such as pet owners, general practice veterinarians and specialists. Definitions of a serious condition versus a non-serious condition, he added, can vary between countries. "It's a very strict, formal process," Goldstein said. "This is not free text."
Still, he accepted that human error may be a factor. "Zoetis takes reports of potential adverse events very seriously and works to better understand adverse event reports and share them with the appropriate regulatory authority," Goldstein said.