Nicole Vumbaco and her faithful companion, Pancake

Photo by Teresa Taylor Vumbaco
Ravaged by an elusive infection she contracted from a cat bite, Dr. Nicole Vumbaco curls on the couch with her trusty companion, Pancake. "I look perfectly healthy, but my body is waging a war within," the veterinarian says.
Despite decades of research and mounting evidence that the infection commonly known as cat scratch disease can cause chronic, systemic illness, those most often affected — veterinarians and others who work in animal care — struggle to be taken seriously by physicians.
For many patients, the illness transmitted by the saliva of infected cats or fleas and other insect vectors causes only temporary, if acute, symptoms. But in some patients, it's an insidious disease that can wreak long-term havoc throughout the body and cause a range of debilitating conditions affecting the heart, nervous system and musculoskeletal system.
Dr. Edward Breitschwerdt, a veterinary internist and one of the world's top experts on Bartonella, the genus of bacteria responsible for cat scratch disease, said the illnesses caused by these bacteria remain mostly an afterthought.
The medical importance of only three of the more than 40 known Bartonella species has been studied, he said, and research into Bartonella is largely unsupported by the National Institutes of Health.
"There has been almost no funding at the federal level," said Breitschwerdt, a professor of medicine and infectious diseases at North Carolina State University College of Veterinary Medicine. "Any new bacteria that comes along probably requires an advocacy group to ultimately convince agencies that it's important enough to put some money in to understand how important it is medically," he added.
The role of Bartonella in chronic illness remains a mystery to most physicians, and the occupational risk of acquiring Bartonella infection often is underestimated by veterinarians and others who work with animals. The prevalence of infection is unknown.
The experience of Dr. Nicole Vumbaco offers a glimpse into the problem. The veterinarian ascribes years of misdiagnoses and her subsequent physical disability and loss of livelihood to the lack of knowledge and under-recognition in the medical community.
It all began on a winter morning in early 2017 while she was working an emergency clinic shift in Colorado, tending to Molly, a shorthaired cat in critical condition.
"She was a known diabetic," Vumbaco, then 34, recounted. Following an insulin injection at home, the cat went into hypoglycemic shock and became unconscious. "She had muscle spasms and lockjaw with oral trauma," said Vumbaco, who treated Molly with oral and intravenous dextrose.
When the cat came to, she bit Vumbaco on the finger. Vumbaco cleaned the wound and later that evening, started a course of antibiotics. That wasn't the end of it — rather, it was the beginning of a prolonged and agonizing journey with a condition that wasn't confirmed until years later as bartonellosis.
A constellation of possible effects
Cat scratch disease was first described over a century ago. But bartonelloses — the term for chronic systemic illnesses caused by Bartonella — were unheard of in North America until a few years into the AIDS epidemic. That's when pathologists and clinicians linked patients' blood-blister-like lesions to two Bartonella bacteria (B. quintana and B. henselae).
B. henselae is the species most frequently identified as the pathogen responsible for cat scratch disease. Breitschwerdt said cats evolved as the adaptive reservoir hosts for the bacterium, meaning they act as a source of the infective agent capable of transmitting it to other hosts. Dogs and coyotes have evolved with another type of Bartonella, and rats and squirrels with still others.
The bacteria are transmitted by vectors including infected fleas, sandflies, lice and keds (a type of fly). In cats, cows, dogs and humans, Bartonella can cause heart conditions, although acute infections in people more typically are associated with fever, headache, exhaustion, short-term memory loss, swollen lymph nodes and poor appetite.
A day after the cat bite, Vumbaco felt flushed. Her heart raced and her finger throbbed. She didn't feel terribly sick, but by mid-morning, a deep red streak traced up her arm. She headed to the hospital, by which time the streak had reached her neck.
She was admitted for a day and given IV antibiotics. Some symptoms of infection eventually improved, while others worsened. She became nauseated and had vertigo, extreme fatigue and difficulty breathing.
About two weeks later, after she'd finished the oral antibiotics, Vumbaco's condition took a marked turn for the worse. "As my symptoms progressed, I said, 'I think I have cat scratch disease,' but nobody shared my concern," she recalled. "I requested 21-day blood cultures and antibody titers but was dismissed over and over again." Her doctors were stumped by her deteriorating condition.
A fellow veterinarian, Dr. Edward Breitschwerdt is the go-to guy on bartonelloses
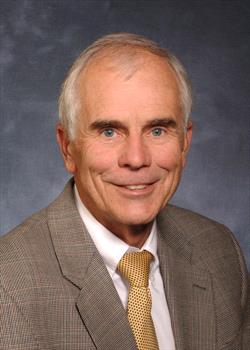
NCSU photo by Wendy Savage
For veterinarians, the go-to expert on detecting
Bartonella bacteria in people is a fellow veterinarian at North Carolina State University, Dr. Edward Breitschwerdt.
"The problem is that Bartonella can cause an acute infection that is most often self-limiting without treatment," Breitschwerdt explained. "It's currently not recommended that physicians treat patients with classic cat scratch disease; in most instances, the fever and lymph node swelling resolve, and it's assumed that the patient's immune system has eliminated the bacteria."
Breitschwerdt's Intracellular Pathogens Research Laboratory at NCSU has been a leading contributor to the worldwide discovery of the more than 40 Bartonella species, and he, with colleagues, has authored more than 40 published papers describing human illness. Breitschwerdt said his and others' research has shown that the pathogen establishes a persistent infection in some patients.
Vumbaco's symptoms ebbed and flowed, but overall, she grew increasingly ill. In the acute period, she developed a rash, muscle and joint pain, shortness of breath, worsening cyclic flu-like symptoms with a low-grade fever, swelling, fatigue and a heart murmur. Doctors thought she was having a delayed reaction to the antibiotic Augmentin and prescribed immunosuppressive steroids.
For months, which became years, Vumbaco continued to suffer an onslaught of inflammatory conditions and other health problems affecting her entire body. She also endured complications from ostensibly simple surgeries. An operation to repair torn cartilage in her hip led to 10 more procedures. A routine root canal led to oral surgery.
Vumbaco saw specialist after specialist, including two infectious diseases doctors, hoping for answers. Conventional lab work failed to identify a culprit. She long suspected that Molly's bite was at the root of her ailments but could not convince doctors to order tests for Bartonella.
"My body was caught in a downward spiral. It was an onslaught of unknown origin," she said. "They still declined my request for testing."
At one point, doctors suspected her problems were induced by stress. By 2019, eight years into her veterinary career, she could no longer work.
Stealthy, slow-growing pathogen
One of the difficulties with detecting Bartonella, Breitschwerdt said, is that "it's not a rapidly dividing bacteria like Staphylococcus aureus or Escherichia coli, and it also hides in numerous cells and tissues. It's more similar to the germ that causes tuberculosis — an intracellular, slowly dividing bacteria that is notoriously difficult to treat with antibiotics.
"If you are a rapidly multiplying bacteria, such as Staphlococcus or E. coli," he elaborated, "you are more prone to die when the patient is given an antibiotic. For an intracellular bacterium like Bartonella with a slow dividing time of 24 hours, those antibiotics are not going to be as effective."
Nicole with Pancake before she got sick

Photo by Dr. Mariel Knox
Before she was infected with
Bartonella in 2017, Vumbaco, shown with Pancake, regularly ran and hiked.
Why Bartonella causes chronic illness in some people is not well understood, but research has shown that people with a compromised immune system — such as those with HIV, undergoing cancer treatment or taking immune suppressive therapy — are at higher risk. Young children, adolescents, older adults and pregnant people also are likely more susceptible. It's also possible that a coexisting chronic viral or bacterial infection makes it harder for the body's immune system to manage the problems that bartonelloses cause.
At age 15, Vumbaco was diagnosed with Hashimoto's thyroiditis, an autoimmune disease that is the most common cause of hypothyroidism in the U.S. The condition did not affect her active lifestyle, which included trail running regularly.
"While prior diagnoses may have made me more susceptible to chronic infection, it doesn't tell the full story," Vumbaco said. "Completely healthy people, with no preexisting conditions or preexisting autoimmune tendencies, can and do acquire bartonelloses."
She believes misguided treatments contributed to her decline. "For me, the most damaging factor was the liberal use of high-dose steroids by treating doctors — in both the acute and chronic period — which suppressed my immune response and allowed this infection to flourish," she said.
The infection ultimately caused central nervous and immune system problems, muscle, joint and tissue disorders, as well as liver, kidney, bladder, heart and lung abnormalities.
"This disease has taken my ability to practice medicine, earn any type of income, my reliability, functional capacity, independence and financial stability," Vumbaco, now 41, said. "It's brought into question my ability to ever have children. It's an incredibly deceiving disease; I look perfectly healthy, but my body is waging a war within."
Two years later, diagnosed at last
Her medical hardships started to ease in 2019 after she reached out to Breitschwerdt, who had developed a novel and more sensitive diagnostic test to detect Bartonella infections in patients with chronic debilitating illness.
The bacteria are difficult to find in human blood specimens, in part because they invade and lurk inside a variety of human cell types and are periodically released into the bloodstream, enabling the infection to travel to new areas of the body, he explained.
Infected cells include erythrocytes, the red blood cells responsible for carrying oxygen to tissues, endothelial cells that line blood vessels, blood and tissue macrophages that defend the body from infection, bone marrow cells and connective tissue cells. Among vector-borne pathogens, Bartonella species are potentially unique in their ability to infect and persist in numerous cells and tissues.
It's been a long haul involving lots of medication

Photo by Dr. Nicole Vumbaco
Vumbaco has consumed many bottles of medication in the quest to conquer her condition. She said her mom came up with an idea of doing "something special every three months with all my empties to quantify progress."
Vumbaco is one of many veterinarians who have reached out to Breitschwerdt in recent years searching for answers to inexplicable health problems. About 1,200 people have been part of his research studies, most of them veterinarians, many of whom complained of neuropsychiatric or other debilitating symptoms.
"There are many, many young to middle-aged veterinarians whose infection data we have published that are identical to Nicole's," he said. Like Vumbaco, he noted, they commonly reported being active and healthy before their condition began to deteriorate. Most had consulted numerous physicians without resolution.
Breitschwerdt's research team improved the sensitivity of tests for B. henselae and other Bartonella species using a unique insect cell culture enriched with various supplements to enhance bacterial growth for easier detection.
Polymerase chain reaction (PCR) tests are used to document the presence of Bartonella species' genetic material.
"Once we detect the DNA of the bacteria in the sample, we can sequence it and say exactly what Bartonella species and strain caused the infection," Breitschwerdt said. "Based upon the cumulative improvements we have made in assay sensitivity over the years, I'm pretty sure we can hit an 80% diagnostic accuracy. We have more work to do to achieve closer to a 100% test sensitivity."
His diagnostic work has grown beyond his university research laboratory to a business he co-founded in 2009, Galaxy Diagnostics, to find Bartonella in animal and human patients missed by other diagnostic laboratories.
Vumbaco enrolled in one of Breitschwerdt's studies, sending samples every other day for three collections, and in February 2020, had her answer. She was blood-culture and direct-PCR-positive for Bartonella on two of the three samples.
"I finally got a diagnosis that explained every aspect of my clinical profile," she said. "I was elated at the chance for recovery."
Prevention and documentation
Step-by-step improvement
One month later, Vumbaco started a gradual and complex treatment regimen beginning with supportive medications, along with hormone replacement therapy and a prophylactic anti-fungal drug to prepare her body for the onslaught of antibiotics she would need. She is on a triple-antibiotic therapy (rifabutin, clarithromycin and Bactrim), along with the other targeted treatments to manage lingering conditions.
Since starting treatment, Vumbaco reported, she's had marked improvement in most of her symptoms, and her heart, lung and liver abnormalities have all resolved. She continues to have chronic fatigue, weakness, numbness, joint pain and neuropathic pain, but on the whole, she says, life is better.
"I am able to walk my dog, Pancake, three or four times a week, and that's been a huge win, especially for my mental health."
For his part, Breitschwerdt, 74, continues his research, now collecting data on the role of Bartonella in neuropsychiatric illness.
With grants from the Cohen Foundation, his team is working to further improve diagnostic sensitivity, and will soon launch a study to test for Babesia, Bartonella and Borrelia species in patients with long Covid. His NCSU research team is also engaged with counterparts at Duke and Tulane universities to develop a targeted treatment for bartonelloses.
"It's an interesting genus," he said, "or I'd be retired by now."