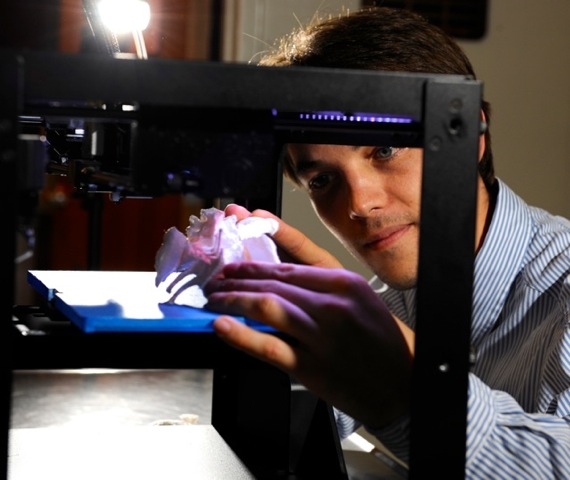
Photo courtesy of Auburn University College of Veterinary Medicine
Testing out the new 3-D printer he obtained for the Auburn University College of Veterinary Medicine with a grant, radiology resident Dr. Adrien-Maxence Hespel examines a model of a dog's pelvis
As a veterinary neurosurgeon, Dr. Don Sorjonen has performed ventral atlantoaxial stabilization — a procedure to repair defects between the top two vertebrae in the neck — on more than 50 animals.
This summer, as he readied for surgery on a 3-pound Yorkshire terrier named Sophie, Sorjonen learned of a way to make the familiar operation go still more smoothly and surely.
A radiology resident at the Auburn University College of Veterinary Medicine in Alabama, where Sorjonen is a professor emeritus of neurology and neurosurgery, offered to make a model of the affected part of Sophie’s cervical vertebrae using a 3-D printer. The life-size model enabled Sorjonen to practice the surgery and obtain the right-size tiny screws and plates he needed for an optimal result.
The debut of 3-D printing at Auburn’s veterinary college is yet another application of a fast-spreading technology that’s being used to make
everything from firearms to toys to clothing to prostheses and more.
Printing in three dimensions for veterinary practice isn’t a new concept. Researchers have published scientific articles about the possibilities for several years. But Dr. Adrien-Maxence Hespel and colleagues are among the first to vigorously promote the technology to clinicians.
Hespel, a second-year radiology resident, said he’d been pondering ways to enhance the use of CT scans. Computerized tomography captures X-ray images of bones and soft tissues in cross-sections that can be combined to give viewers a 3-D perspective on a computer screen. But that’s not truly 3-D, and examining different aspects of an image requires manipulating it on a computer.
“I thought it would be so great to be able to print that (3-D image) and give it to the surgeon. They would be able to take it, like a pen or a key or whatever, and turn it around and see how things are,” said Hespel.
He envisioned models as a helpful tool for communicating medical information to clients, as well. “You could try to explain, ‘Your dog has a tumor from this area,’ and they might just look at you blind,” Hespel said. “You need to come up with an illustration; a way for them to apprehend the pathology.”
So when his college’s Information and Instructional Technology Committee offered technology grants, Hespel, with support from his mentor, radiologist Dr. Judith Hudson, applied. The project won $6,000.
The sum easily covered the machine, a Makerbot 3D printer, which Hespel said cost $2,500 including an extended warranty. Software is the more expensive portion. The program he sought was priced at $11,000. Fortunately, an anatomy professor at the veterinary school had a copy for making 3-D book illustrations, enabling Hespel to obtain access less expensively.
Then he had to work out the process of moving a CT image from the computer onto the printer. “Nobody tells you exactly what the secrets are to get from a CT to a plastic model,” Hespel said. “That was a big jump for me, to go from something on the screen to something understandable by the printer.”
The process entails running the images through two different computer programs taking care to maintain the proper proportions and not introduce artifacts to the model.

Photo courtesy of Auburn University College of Veterinary Medicine
Sophie, a young 3-pound Yorkshire terrier, was the first patient at Auburn to benefit from the veterinary college's capability to make 3-D models.
Sophie, the Yorkshire terrier, was the first patient at Auburn to benefit from the college’s new equipment.
The tiny dog was born with malalignment and instability of the first and second cervical vertebrae, which subsequently compressed the spinal cord, a painful and disabling condition. Though not completely paralyzed, she could not stand or walk on her own.
The surgical solution was to realign the vertebrae, using a plate and screws to maintain the alignment and stabilize the joint, then fuse the bone. The delicate procedure is particularly challenging in a 3-pound animal.
“Because of Sophie’s small size and the bones that we have to realign and fuse, it was very helpful to have an exact model of the instability, or the pathological area, in my hand,” Sorjonen said.
The model enabled him to make accurate measurements in order to know the exact plate and screw size needed, he said. “When we went in surgically … it was just a matter of replicating the model procedure in the animal.
“The accuracy of the reproduction, that was the most astounding thing to me,” Sorjonen continued. “I did not see any variables between what we did on the model and what we did in the animal. Everything fit up exactly. The plates were probably a little over one centimeter in length; the screws were four to five millimeters long. Therefore, we (did) not have much room for error.”
As co-designer of the ventral atlantoaxial stabilization procedure, Sorjonen had been comfortable performing the operation without benefit of a practice model, but it required a certain degree of resourcefulness.
“You never know what you’re going to encounter,” he said. “In some dogs, we have made decisions table-side, so to speak. … We may not have the right equipment, so we sometimes put in a series of pins and screws just to hold the dog until we find something else we can use.”

Photo courtesy of Auburn University College of Veterinary Medicine
With this model of one of Sophie’s vertebrae, a surgeon was able before surgery to obtain precisely right-sized plates and screws to correct a malalignment.
With the 3-D model, he said, “I knew exactly what I was up against before I got there. I knew exactly what type of equipment I needed. … It’s wonderful. I’ll never do it any other way now that I have this option available to me.”
Another patient to benefit from the 3-D modeling was Solo, a 6-year-old horse who suffered a devastating facial injury in October. The bone around his right eye was shattered, possibly from being kicked by another horse.
Dr. Fred Caldwell, an associate professor of equine surgery, described the injury as “an extremely comminuted orbital fracture. The bone was broken into multiple pieces and kind of pushed inward.” Caldwell explained that horses have large sinuses, behind which is little bony support. “When they take a blow to the area, it just crushes everything. … I’ve seen some of these in the past,” he added, “but … (not) one as severe as this.”
Because Solo is a competitor in equestrian sporting events, it was important to save his eye, Caldwell said.
He recommended to the horse’s owner doing a CT scan as a way of identifying the locations of the multiple fracture lines. When Hespel offered to create a 3-D model from the CT image, Caldwell enthusiastically accepted.
“I spent a lot of time with that model, I tell you,” he said. “I took it home the night Adrien made it.”
Caldwell said studying the model enabled him during the operation to be more precise with incisions and to move bones back into place more efficiently. “I would hazard a guess that it cut the surgery time almost in half,” he said, “probably (reducing the time) from three hours to an hour and a half.”

Photo courtesy of Auburn University College of Veterinary Medicine
Solo needed two surgeries to repair catastrophic fractures around his right eye.
Solo's surgeon credits advance planning using 3-D
models for making the operations go more quickly and smoothly.
For patients in general and for horses in particular, the less time spent anesthetized, the better. “Since they’re so large and lying on a table, they’re compressing their muscles. They may not perfuse very well under anesthesia. They can have problems standing back up again,” Caldwell explained.
As the swelling on Solo’s face eased, Caldwell planned a second surgery to better position the eyeball. “We ended up doing a second CT about three weeks later, and we could see an area where there was a bone that was still kind of displaced. Adrien created another 3-D model … and I was able to see exactly what we needed to do to go back in on the sinus side and get the eyeball back into a more normal position,” he said. “The amazing thing to me was, what I was seeing on the model was exactly what we saw when we went into surgery.”
Today, Solo is back home, his eye intact and able to see.
The value of 3-D models for surgery preparation is greatest with complex or unusual cases. “What the technology allows us to do is to plan,” Sorjonen said. “Some procedures are routine enough that we really don’t need that much pre-surgical planning; we just go in and do it.”
Creating a model can be expensive because it requires an MRI or CT scan, imaging that may cost upward of $1,000. But in situations for which such imaging already is needed, the price of a 3-D model is negligible. The material used is an inexpensive plastic called polylactic acid, Hespel said, estimating the cost of a single model at $3 to $5.